Exercise-induced bronchoconstriction (EIB) is a hallmark of asthma and other respiratory diseases. It occurs when vigorous physical activity triggers transient and reversible airway narrowing. Environmental factors such as cold, dry air and air pollution are known to exacerbate symptoms, particularly in athletes and individuals exercising in urban environments.
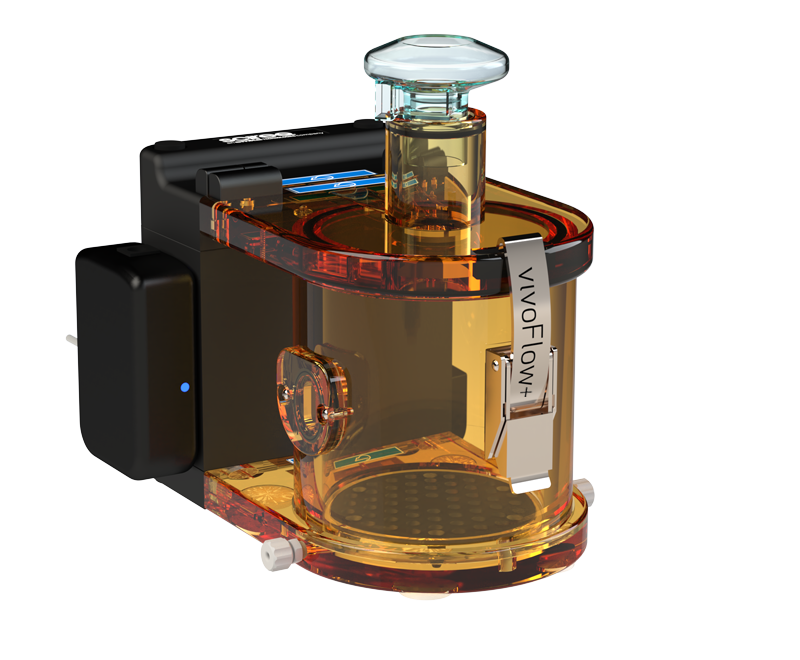
A recent study by Marain et al. (2025) develops a murine model to investigate the combined effects of cold air, diesel exhaust particles (DEP) and exercise on lung physiology and airway inflammation. By integrating SCIREQ’s flexiVent and Double Chamber vivoFlow+ Plethysmography, the group captures both non-invasive breathing patterns and invasive, high-resolution lung function outcomes. These complementary approaches provide new insights into the pathophysiological mechanisms underlying exposure-associated EIB.
Novel Model for Exposure-Associated EIB
BALB/c and C57BL/6 mice were divided into eight groups based on three conditions:
- Exercise vs. rest
- Room temperature vs. cold air (4 °C)
- DEP vs. saline exposure
BALB/c mice emerged as the more responsive strain, exhibiting significant bronchial hyperresponsiveness (BHR) and neutrophilic inflammation after cold air exercise, while C57BL/6 remained comparatively resistant. This finding establishes BALB/c as the preferred model for exposure-associated EIB studies.
Breathing Pattern Analysis
Non-invasive measurements with Double Chamber Plethysmography (DCP) revealed that cold air and exercise profoundly alter respiratory rhythm:
- Expiratory time is prolonged.
- Breathing frequency decreases, particularly in the Saline + Exercise + 4 °C
- End-expiratory pause (EEP) increases only in the DEP + Exercise + 4 °C
These findings demonstrate that cold air alone modifies breathing behavior, while DEP intensifies airway obstruction during exercise.
Lung Function Measurements
The flexiVent FX system provided high-resolution data on lung mechanics 24 hours after the final exercise session.
- At the highest methacholine dose (40 mg/ml), both the Saline + Exercise + 4 °C and DEP + Exercise + 4 °C groups developped pronounced bronchial hyperresponsiveness, characterized by a significant rise in airway resistance (Rn) and a marked reduction in %FEV₀.₁.
- Small airway resistance reached its peak in the DEP + Exercise + 4 °C group, indicating that the combination of cold air, exercise and diesel exposure exerts the most severe impact on airway function.
Inflammation and Epithelial Injury
- A significant neutrophil influx was observed in the bronchoalveolar lavage (BAL) fluid when cold air, DEP and exercise were combined.
- Diesel uptake by macrophages increased, with the highest load in the DEP + Exercise + 4 °C
- Epithelial damage was indicated by surfactant protein D (SpD) leakage into serum, which was observed in diesel-exposed exercising animals, whereas exercise or cold air alone did not cause significant leakage.
These outcomes show that environmental stressors not only alter lung mechanics but also trigger pro-inflammatory and tissue-damaging responses in the airways.
Implications and Conclusion
This study establishes a reproducible murine model of exposure-associated EIB, demonstrating that the combination of cold air, exercise and DEP induces the most severe airway dysfunction, inflammation and epithelial injury. By combining flexiVent FX and Double Chamber Plethysmography, the model links altered breathing patterns with mechanistic measures of airway resistance and inflammation, bridging the gap between functional outcomes and underlying pathology.
The findings highlight the risks of exercising in cold, polluted environments, where exposure significantly increases the likelihood of airway narrowing and inflammation. This has important implications for athletes, outdoor workers, and patients with asthma or chronic respiratory diseases. At the same time, the murine model provides a valuable platform to test therapeutic interventions and to develop preventive strategies aimed at reducing the impact of environmental triggers on respiratory health.
References
Marain, N. F., Dilissen, E., Cremer, J., Vanstapel, A., Bullens, D. M., Dupont, L. J., & Vanoirbeek, J. A. (2025). Cold air and air pollution induce bronchial hyperresponsiveness and inflammation in a murine model. Science of the Total Environment, 989, 179828. https://doi.org/10.1016/j.scitotenv.2025.179828
Featured Product
Empowering researchers
Welcome to SCIREQ’s knowledge center. You can find everything from software registration to document downloads to complete list of SCIREQ publications in this section. Everything you need to get the most out of your SCIREQ system.